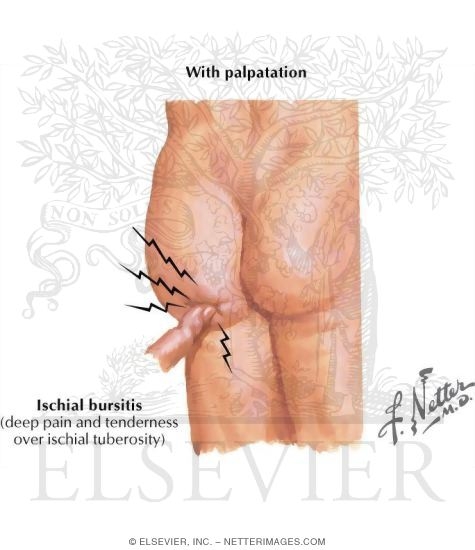
There are two types of hip bursitis. Ischial Bursitis which is a swollen bursa near where your hamstring attaches on your Ischial Tuberosity (SITS bone) and Trochanteric Bursitis which is where your Gluteal muscles attach on the greater trochanter located on the side of your femur. Bursitis can occur for many reasons such as direct blunt trauma to the region or repetitive motion which causes the tendon to compress the bursa leading to swelling and pain. I see and treat hip bursitis regularly at my office and over the years have developed a “sixth sense” in recognizing it and treating it effectively. Unfortunately for many patients they have seen doctors or therapists who do not recognize it and think it is a muscle issue. This results in poor patient management and aggravation of their problem. A bursa is a fluid filled sack that’s purpose is to prevent friction between the tendon and bone. You can not stretch it or strengthen it. In fact, this approach usually serves to aggravate it. Cortisone can be a highly effective intervention but it is important to understand that cortisone is not “magic”. It is a powerful anti-inflammatory agent that degrades inflammatory enzymes and can be used to interrupt the inflammatory cycle. If the patient is not educated or counseled on WHY they developed the bursitis and the offending activity is not removed or modified the cortisone injection will either be ineffective or temporary at best. A perfect example of this would be a runner with hip bursitis. They tell the doctor that it hurts to run, especially up hills. The doctor injects them with cortisone and tells them to stretch it. The runner goes home, OVER-STRETCHES their hamstring and then goes for a run up the side of their favorite mountain. The over-stretching causes their hamstring tendon to strain and the running compress their bursa. Later they are in more pain than before they received the injection and think it did not work. The real issue is they were not managed properly by the doctor either due to ignorance or apathy on the doctor’s part. Of course it is also possible they were misdiagnosed or the doctor failed to hit the mark and actually inject the bursa…..but let’s ASSume competence on the doctor’s part. The following is a real story about a patient that presented to my office recently and her 2 years of misery and butt pain due to the lack of guidance and education about her bursitis condition.
A woman presented to my office complaining of pain in her gluteal region for two years. She explained that it hurt to sit and walk uphill. Her medical history was extensive. She had MRI’s and X-rays for me to review. After reading her MRI report I knew there was at least 2 “smoking guns” that could be responsible for her issue. The MRI showed Ischial Bursitis AND a bulging disc in her lower lumbar spine. Bulging discs can compress nerves. Pinched nerves can cause pain in areas far removed from the pinch site. This often results in the patient thinking they have s muscle problem and confusion on the doctor’s part because they are trying to diagnose something at the site of the patient’s pain. After listening to her horrible saga and litany of procedures that had been done to her I began a series of provocative tests that would help me determine the true source of her pain. Through orthopedic testing I was able to rule out a pinched nerve (Sciatica) and other conditions like Piriformis Syndrome, Gluteus Medius Syndrome and High Hamtring Tendonopathy (HHT). She explained that sitting made it worse. I rolled up a towel and had her place it under her hip. This served to elevate her bad hip so that it was not touching the chair but in effect was “floating”. I saw the smile spread across her face. “That really helped”, she said. “Right”, I replied. “Without the pressure on your SITS bone the bursa is not being compressed so it feels better”. This knowledge coupled with her MRI findings and a few other variables allowed me to confidently tell her she was suffering from Ischial bursitis. Once she realized that pressure was the offensive variable she told me how she often sees a massage person that “really gets in there and breaks things up” by putting her elbow into the women’s Glute and applying terrible pressure. The patient told me how she feels worse after seeing this massage person but thought that it was suppose to hurt! She also told me how her neighborhood has lots of hills and she walks them daily even though it aggravates her hip problem. To my surprise she also told me that I was the first doctor to actually touch her, find the source of her pain, educate her regarding the problem and provide her with a written treatment plan which consisted of home exercises, treatment recommendations and activities to avoid such as walking up hills. My explanation of how to sit using the rolled up towel made her especially happy because she felt immediate improvement.
I am confident that she will improve quickly because I helped her remove the offending variables that were actually aggravating her condition. Unfortunately there are many doctors and therapists out there who do not recognize or know how to properly manage Ischial Bursitis. Doctor means “Teacher”. Yes they may have a medical degree but for whatever reason never learned how to properly manage this condition. A Doctor’s job is to find the source of your problem, remove it and teach you the do’s and don’ts so that you can recover. Take this scenario. You begin to have pain in the bottom of your foot. It only seems to hurt when you wear a certain pair of shoes but it is your favorite pair. You go see the doctor and he/she diagnosis you with “footitis” then injects you with cortisone and puts you in a walking boot for 4-6 weeks. Your foot actually feels better and after 4 weeks you start wearing your favorite shoes again. To your dismay the pain returns to your foot. You decide to make an appointment with my office and the first thing I do is inspect your shoe. I find a rock under the shoe insole stuck exactly where your pain is (by the way this actually happened once….no shit) and I remove it. You put the shoe back on and……presto the pain is gone. Why? Because I removed the rock that was causing your pain! In the case above the women had many “proverbial rocks” such as sitting, walking up hills and a massage person who thought inflicting pain on an already painful bursa was a good idea!
It is all too common that patients are being guided by people with good intent but ignorant (to their condition)! In an effort to help themselves they are often aggravating and prolonging their misery! The reason we are wired to feel pain is so that we can avoid it! If you are doing something for your hip bursitis or some other condition and it is painful and making the condition worse STOP IT! Think it through and remove the “rocks”. Use your own judgment and listen to your body. They say the problem with common sense is it ain’t that common! Use your common sense and don’t listen to these misguided people that are leading you down a path of misery.
If you have any questions feel free to email info@sdri.net or to schedule an appointment call 858-268-8525
For more information on Ischial Bursitis click here
The medical information on this site is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be patient education, does not create any patient-physician relationship, and should not be used as a substitute for professional diagnosis and treatment.
Thank you Dr. Runco! Can you please explain in more detail how to use the rolled up towel to release pressure while sitting? Is the towel placement perpendicular to the spine or parallel?
Thanks!
Amy
while sitting raise the affected side knee towards the ceiling. Take the rolled up towel and place it under your thigh just in front of the SITS bone. Lower your knee back towards the ground. You should feel like the affected SITS bone is “floating”